We offer state-of-the-art, evidence-based and patient-orientated treatments and diagnostics for all acute and chronic cardiovascular diseases. This spectrum includes coronary heart disease, heart valve defects, cardiac insufficiency, cardiac arrhythmia, cardiomyopathies, myocarditis, the diagnosis of unconsciousness, high blood pressure and the preparation and aftercare of cardiac surgery. In addition, aftercare is provided for pacemakers, ICD and CRT systems.
Of particular importance at this point is not only the diagnosis and treatment of cardiovascular diseases that have already occurred, but also the importance of preventing these diseases from developing in the first place or rather diagnosing them at a very early stage so that a decisive influence can still be exerted on their progression. This area of cardiology is known as cardiovascular prevention and is becoming increasingly important.
More information: cardiovascular prevention
Frequently asked questions (FAQs)
Coronary heart disease (CHD) - How does a heart attack occur?
The most common cause of a heart attack is a narrowing of the coronary arteries, known as coronary heart disease (CHD). It is the result of arteriosclerosis (vascular calcification), which can occur in all blood vessels in the body and most frequently affects the coronary arteries. These deposits consist of fat (cholesterol), which calcifies as it progresses, causing the vessels to harden and narrow.
If there is no longer enough blood flowing through the coronary vessels, the heart muscle can no longer be supplied with oxygen. Even at this stage, chest pain (angina pectoris) can occur as a result of exertion. However, this does not always have to be the case. Often the first symptom is only shortness of breath on exertion or shortness of breath (dyspnoea).
If the blood flow in a coronary vessel is completely interrupted so that blood can no longer flow through it, a heart attack occurs. This can be characterised by persistent, belt-like tightness in the chest and shortness of breath, even at rest, and requires immediate treatment with a cardiac catheter.
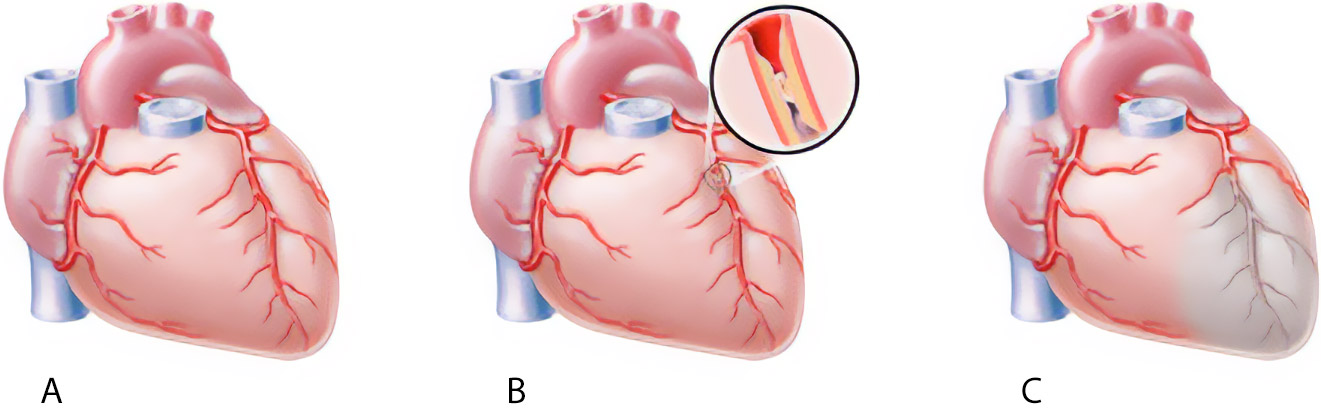
© DHS / medicalArtworkMainz
A: The blood flows normally
B: The blood flow and thus the supply of oxygen to the heart muscles is interrupted
C: Closed vessel
What are the signs of an acute heart attack (acute coronary syndrome)?
The process of arteriosclerosis is gradual and often begins decades before the typical symptoms such as chest pain and/or shortness of breath appear. These symptoms first occur under physical or emotional strain (stress) before they become noticeable at rest.
Look out for the following signs:
- Severe pain and a feeling of pressure in the chest
- Massive tightness
- Shortness of breath
- Severe burning sensation
- Back pain
- Cold sweat, cold and pale skin
- Nausea, vomiting and pain in the upper abdomen
- Drop in performance
In this case, call 112 immediately. Every minute counts!
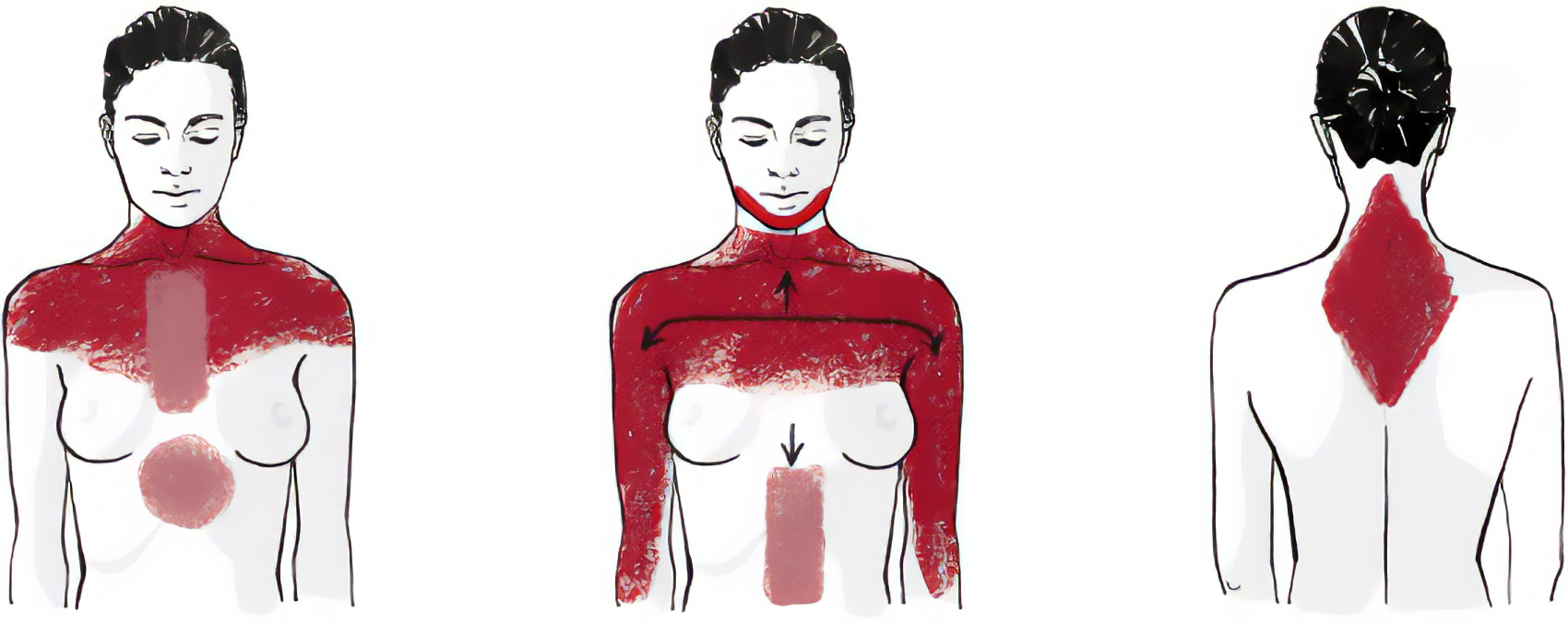
Do the symptoms of a heart attack differ between women and men?
In contrast to men, the typical symptoms mentioned above are often less pronounced in women and are therefore underestimated.
Although heart attacks occur later in women compared to men (on average ten years after the menopause), they have a poorer chance of recovery after surviving a heart attack compared to men. It is therefore particularly important for women to have their symptoms checked immediately.
However, younger women before the menopause should also take symptoms seriously. If the above-mentioned risk factors for arteriosclerosis are present together with a genetic risk (i.e. heart attacks, strokes in first-degree relatives or siblings before the age of 60), the utmost caution is also required here.
How is a heart attack treated?
Every second counts in the event of a heart attack. The faster a blocked coronary artery is reopened, the greater the likelihood that no long-term consequences such as cardiac insufficiency or cardiac arrhythmia will remain. The gold standard in such situations is a cardiac catheterisation, which can be used to reopen coronary arteries by means of a balloon and the placement of a stent. This allows the heart muscle to receive sufficient oxygen to regenerate.
To ensure that a stent remains open after a cardiac catheterisation and does not close again, blood-liquefying medication must be taken permanently. In addition, the risk factors that have contributed to the development of vascular calcification are optimised with further medication in order to prevent future recurrences (secondary prevention). This requires regular check-ups with your cardiologist.
Occasionally, the situation arises in which the coronary arteries are constricted in such a high number and unfavourable localisation that the implantation of vascular supports (stents) is no longer possible or sensible. In such cases, bypass surgery is the only way out.

© herzmedizin.berlin
What are the risk factors for the development of arteriosclerosis?
The main risk factors for arteriosclerosis and therefore coronary heart disease are obesity, high blood pressure, diabetes, high cholesterol levels, smoking and lack of exercise.
Age is also a risk factor in its own right. In addition, a genetic predisposition to heart attacks or strokes in the family can exacerbate all the risk factors mentioned and accelerate arteriosclerosis many times over.
In the presence of such constellations, regular consultations with your cardiologist are of crucial importance in order to optimise the risk factors as much as possible. The first step is to provide appropriate counselling regarding lifestyle changes and the second step is to take medication if necessary.
How often are check-ups necessary for coronary heart disease (CHD) or after a heart attack?
Regular cardiological follow-up checks are of crucial importance and should take place every six months. At these check-ups, echocardiography and stress tests are used to check the blood flow in the coronary arteries.
In addition, the medication is checked on the basis of blood values (cholesterol, blood sugar) and adjusted if necessary.
How is heart failure defined and how does it develop?
Heart failure is not a disease in its own right, but is usually the result of a pre-existing cardiac condition. Depending on which side of the heart is more affected, it is referred to as right or left heart failure. The most common reason for this is coronary heart disease (CHD), in which narrowed coronary arteries lead to circulatory disorders in the heart muscle, which in turn lead to an impairment of the pumping capacity of the heart muscles. This subsequently results in cardiac insufficiency.
However, high blood pressure can also lead to heart failure, especially if it has been present for many years and has not been adequately treated. This leads to a thickening of the heart muscles, making them less elastic so that they can no longer fill with enough blood. As a result, the heart loses its pumping capacity. High blood pressure is therefore the most common cause of diastolic heart failure.
If heart valves no longer close or open properly, this leads to an increase in pressure in the heart cavities, which can also lead to enlargement of the heart chambers over time and result in a reduction in cardiac output and therefore heart failure.
Another reason for heart failure is inflammation of the heart muscle (myocarditis). These are often the result of a past viral infection. If the inflammation is diagnosed and treated too late, it can result in damage to the heart muscles. This is often the case in young people if, for example, an infection has not been cured long enough.
In addition to the causes mentioned above, there are also genetic heart muscle diseases (cardiomyopathies) as well as cardiac arrhythmias (e.g. atrial fibrillation), which can trigger heart failure. Other possible triggers can be diabetes mellitus, long-term alcohol consumption, drug abuse or certain medications (mainly chemotherapeutic agents).
What symptoms are associated with heart failure?
Cardiac insufficiency usually begins gradually with an increasing reduction in physical resilience. This is accompanied by progressive shortness of breath, which increases over time and is accompanied by water retention in the lower extremities.
In addition, an accelerated pulse and breathing, coughing and rattling noises, cold fingers and feet and the urge to urinate at night are often noticed.
How is cardiac insufficiency treated?
The first step is to treat the underlying disease, such as coronary heart disease, blood pressure control, etc. In the second step, medication is used to relieve the strain on the heart and thereby support and improve cardiac performance. Cardiac support systems such as a CRT system, with which the contraction processes of the heart muscles can be improved using several probes on the heart, also serve to improve cardiac performance.
Only in very severe cases does a heart transplant or an artificial heart remain as the final form of therapy.
Telemedicine
Heart failure can be diagnosed and monitored during the course of treatment by means of an ultrasound examination of the heart as well as an ECG and special laboratory parameters (BNP). Using special telemedical applications, which we also offer, heart failure can also be closely monitored and therapeutically controlled remotely. This is made possible not only by video consultations, but also by telemedical procedures for optimising therapy control in patients with heart failure.
By regularly recording specific vital parameters of patients in their home environment, these parameters are transmitted via a cloud solution, so that constant monitoring of our patients' state of health is possible regardless of where they are.
How do heart valve diseases manifest themselves and how can they be treated?
100,000 actions per day!
Our heart is a high-performance engine. It pumps blood through the body without pauses - every day, for a lifetime. For it to work, it needs many different components, including the heart valves. They ensure that the right amount of blood flows through the heart and are responsible for ensuring that the blood only flows in the intended direction. In other words, either into or out of both ventricles. At 70 beats per minute, each individual heart valve therefore performs around 100,000 actions per day.
Over the course of a lifetime, healthy heart valves can lose their functionality. For example, they can become narrower due to calcification so that blood can no longer flow sufficiently through them. In this case, we speak of valve stenosis (e.g. aortic valve stenosis). In contrast, heart valves can also become leaky after inflammation, for example, so that blood flows back in the opposite direction. This is referred to as heart valve insufficiency (e.g. mitral valve insufficiency).
Our heart is able to compensate for valvular heart disease over a long period of time using highly complex mechanisms, so that there are no symptoms for a long time. As soon as the first symptoms such as breathlessness, reduced performance, exercise-induced dizziness or water retention in the lower extremities appear, these compensatory mechanisms reach their limits and indicate the seriousness of the condition.
Therapy
For the first time, unfavourable pressure conditions in the heart cavities can be positively influenced by new medicinal approaches. Should the heart valve disease nevertheless progress, depending on the heart valve disease, heart valves can nowadays be replaced minimally invasively via the groin or repaired using clips, in addition to classic open heart surgery, under certain conditions.
After every heart valve operation, regular cardiological follow-up by echocardiography and review of the optimal medication is of crucial importance.
What options are there for detecting cardiac arrhythmias?
Irregular heartbeats can be completely normal - especially if they only occur briefly. However, if they last longer and are accompanied by symptoms such as inner restlessness, anxiety, dizziness or nausea, they may be relevant cardiac arrhythmias that should be clarified by a cardiologist.
In young people, stress and stimulants such as alcohol, nicotine or coffee are often the main causes of cardiac arrhythmia. With increasing age and accompanying risk factors such as high blood pressure, the most common cardiac arrhythmia is atrial fibrillation or atrial flutter. These are considered to be one of the main causes of strokes. The higher risk of suffering from coronary heart disease in old age can also lead to life-threatening cardiac arrhythmias such as ventricular tachycardia / ventricular fibrillation. Functional disorders of the thyroid gland and the mineral balance can also have an unfavourable effect on cardiac arrhythmias or even trigger them in all age groups.
Recording an ECG is crucial for the diagnosis of cardiac arrhythmia in order to be able to select the exact therapy. It is not always possible to have such an ECG recorded immediately. In such cases, a long-term ECG can be performed, which can be carried out for up to seven days.
Thanks to the further development of smart watches and wearables, it is now at least possible to record rhythm documentation in sufficiently good quality to allow diagnosis and thus therapy. We support the use of such technical aids, as they increase the probability of capturing cardiac arrhythmias in everyday life, especially in the case of rare rhythm abnormalities, so that they can be forwarded to us for further evaluation. This has already enabled us to detect many cardiac rhythm events without patients having to come to the practice for an ECG.
The use of the latest technologies in diagnostics and therapy for all heart diseases and primarily cardiac arrhythmias is being continuously advanced at the German Medical Centre in collaboration with medical device manufacturers.


